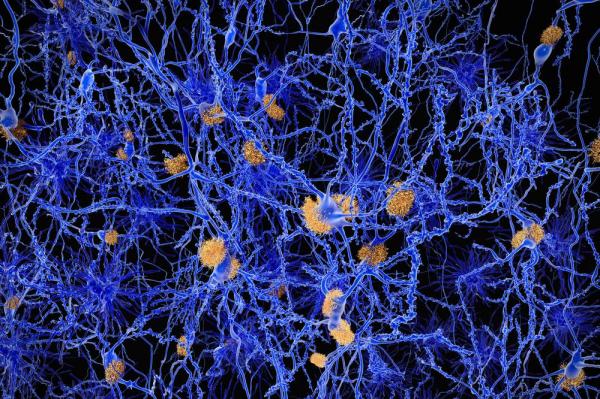
BOSTON, May 26 (UPI) — The build-up of plaques in the brain believed to cause Alzheimer’s disease may be part of the innate immune response to bacterial infection, which scientists say completely changes their understanding of the disease’s development.
Scientists at Harvard University found amyloid plaques believed to be a primary cause of the neurodegenerative disease are not simply waste stuck in the brain, a finding they cautiously say may explain the disease and point the way toward treatment and prevention.
“Our findings raise the intriguing possibility that Alzheimer’s pathology may arise when the brain perceives itself to be under attack from invading pathogens, although further study will be required to determine whether or not a bona fide infection is involved,” Dr. Robert Moir, a researcher in the genetics and aging research unit at Massachusetts General Hospital, said in a press release.
“It does appear likely that the inflammatory pathways of the innate immune system could be potential treatment targets.”
In a previous study, Moir and Dr. Rudolph Tonzi found amyloid-beta inhibited the growth of pathogens, leading them to develop a theory that plaques in the brains of Alzheimer’s patients could be the remnants of past battles of their immune systems.
To test the theory the new study, published in the journal Science Translational Medicine, the researchers introduced salmonella to the brains of mice with and without the ability to express human amyloid-beta.
The mice that could not make the substance died of the infections, while ones that could express it survived longer. The same was true for roundworms and cultured human brain cells.
The researchers think pathogens may enter the brain through parts of the blood-brain barrier that weaken with age — the hippocampus, where Alzheimer’s disease starts, being the first to weaken — which leads to an immune response and the slow build-up of plaques left over from killing invaders.
Stopping amyloid-beta build-up should no longer necessarily be the only focus of Alzheimer’s studies, the researchers say, suggesting instead that a further understanding of the immune response in the brain and how to stop it would be much more effective against the disease.
“While our data all involve experimental models, the important next step is to search for microbes in the brains of Alzheimer’s patients that may have triggered amyloid deposition as a protective response, later leading to nerve cell death and dementia,” said Tonzi, director of the genetics and aging unit at Massachusetts General Hospital.
“If we can identify the culprits — be they bacteria, viruses, or yeast — we may be able to therapeutically target them for primary prevention of the disease.”






